Once Bitten
Fighting Dengue Fever in Key West and San Juan
By Laura Kolbe
Illustrations by Victo Ngai, Haisam Hussein
Sharp first became an officer of the Center for Disease Control and Prevention (CDC) through its Epidemiology Intelligence Service, a cadre of “disease detectives” created in 1951 to combat the threat of bioweapons in the Korean War. He is now a commissioned CDC officer through the US Public Health Service Commissioned Corps, a service established by Congress in 1889 to fight the recurring epidemics of cholera, yellow fever, and other infectious diseases that ravaged the country before modern sanitation and medicine. The interests of the US Public Health Service have generally aligned with those of the enfranchised American public, and that’s often been a good thing: The Public Health Service helped prove that smoking was tied to early mortality, that the organ-failure syndrome known as pellagra came from niacin deficiency, and that AIDS came from HIV. Those same interests of the enfranchised have sometimes been morally and physically catastrophic for more vulnerable populations, such as the black sharecroppers who participated in the Public Health Service’s Tuskegee syphilis experiment, which from 1932 to 1972 observed the ravages of end-stage syphilis long after a penicillin cure was widely and cheaply available. Though the days of such outright abuses are thankfully gone, Puerto Rico’s liminal status with regard to the American mainland leaves it exposed to the possibility of neglect, fickle funding, and the bureaucratic tangles that arise when a semiautonomous but nonsovereign commonwealth tries to work with the federal government and its manifold agencies.
Sharp grew up in Ohio and did the bulk of his undergraduate and graduate studies in Ontario and Texas, focusing on the molecular mechanisms behind viral infections before he realized he wanted to be a step closer to health care’s front lines. He’s lived in San Juan for nearly six years and speaks English with the slightly lead-footed r’s and toasted vowels of a native Spanish speaker. He likes to quote John F. Kennedy’s 1962 State of the Union address—“The time to repair the roof is when the sun is shining”—when explaining the vigilance that befits a public health officer, however reassuring the island’s tally of official case reports in a given week. He’s in a delicate position, since he and his fellow “feds” assist and collaborate with the Puerto Rico Department of Health at the pleasure of the island’s Secretary of Health, who extends formal written invitations for each CDC endeavor. As administrations and priorities change on the island, CDC officers do their best to defer and keep pace.
Sharp’s nemesis, perhaps public enemy number one of the CDC in Puerto Rico, is the Aedes aegypti mosquito. Aedes aegypti is a domestic animal as beautiful as the housecat—petite among mosquitoes, with dappled legs and a distinctive white “lyre” on its back—and as hardy and reviled as the cockroach. Its peculiar hungers and habits contribute to its frightening success in carrying dengue, chikungunya, West Nile virus, and Zika virus from one human to the next: Unlike other mosquitoes, it eats by day and on the run, able to keep up with a moving ankle and take multiple bites as it goes. It can also graze on a roomful of people in the course of a “blood meal,” depositing countless virions in minutes. Preferring dense human settlements, most stay within 100 yards of home for their two- to four-week life spans, unless home happens to be mobile—Aedes has a notable affinity for the warm, damp innards of rubber tires, part of the reason it has migrated so successfully around the world, from one hub of transportation or shipping to another.
Aedes garners the most attention when the diseases it carries threaten people of relative privilege and agency: savvy, literate people who vote, pay taxes, and have come to expect commensurate protections from the academic and medical institutions that members of their middle classes fund, staff, and run. The physician-officer Walter Reed may well have found outlets for his genius wherever he went, but his discovery in 1900 that Aedes aegypti caused yellow fever certainly had amplified effect because his work served American military interests in Washington, DC, and in Cuba. More recently, the Zika virus, discovered in the 1940s, was shown to correlate with neurologic disease in Polynesia in 2013 and with microcephaly in rural Brazil in the early autumn of 2015, but it is arguable that only the dawning realization of its implications for global travelers and a multibillion-dollar Olympics have brought the public health discussion to fever pitch. While Zika was barely discussed during my first visit to Puerto Rico in October, Sharp now says that “microcephaly and other birth defects caused by Zika virus infection of pregnant women are of paramount concern” to the CDC and the Puerto Rico Department of Health. On May 13, 2016, the CDC redirected an additional $25 million—over and above the $60 million allocated earlier this year—toward Zika preparedness in fifty-three American states, cities, and territories. The Senate approved an additional $1.1 billion in federal spending on the virus on May 17, though the House of Representatives still hopes to whittle this figure in half.
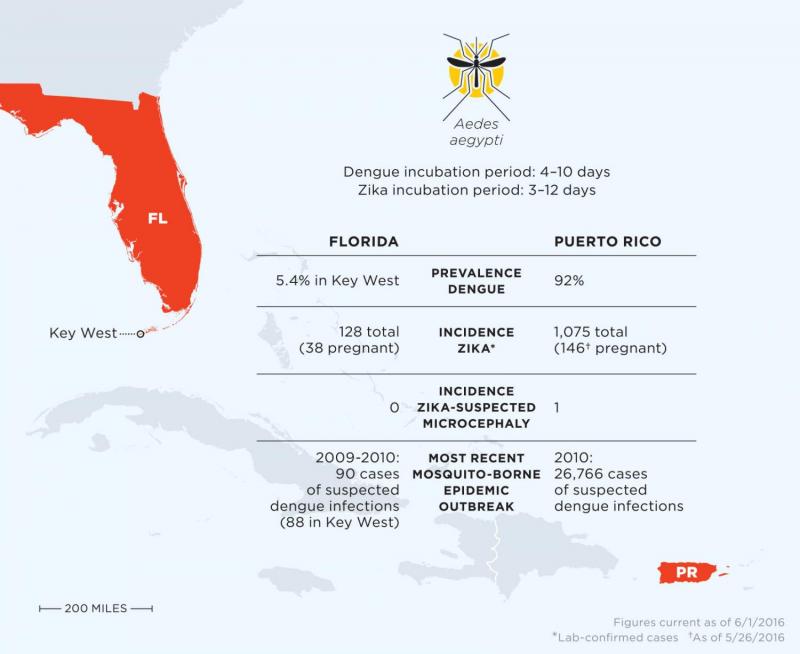
Before the world reacted to Zika—before the FDA ordered a halt to blood donations in Puerto Rico for more than a month this spring, before the World Health Organization told travelers to practice safe sex for “at least” four weeks after travel to Latin America (a number perhaps more troubling for having no certain upper limit), and before El Salvador’s Ministry of Health warned women to avoid pregnancy until 2018—Aedes was wreaking havoc through the transmission of dengue fever, which inflicted decades of morbidity and mortality around the globe to far less attention from the US and other developed nations. Two hundred sixty-four cases of dengue on the Big Island of Hawaii caused a brief media splash in the winter of 2015–16. Before that, if you’d heard at all about American dengue cases, you’d likely heard about the startling isolated case in Long Island in 2013, or heard it on the laundry list of worrisome things allegedly carried across the border with undocumented immigrants. (A 2005 Brownsville, Texas, outbreak of a scant twenty-five cases occurred across the river from 1,251 cases in Tamaulipas, Mexico, suggesting a minimally bug-porous border.) Or else you heard about Key West, where a 2009–10 outbreak of eighty-eight cases roiled the city and led to intense international discussion over whether genetic modification of the mosquito population was a sensible and permissible public health measure.
Comparatively little attention has been paid to the endemic dengue problems of Puerto Rico, which has experienced hundreds of thousands of reported cases in the past fifty years, far more than any other US state or territory. In this dense, complex American territory, dengue has quietly smoldered and flared since 1963. Whether global concerns about Zika—or the next threatened pandemic, wherever it might arise—will ultimately lead to improvements in the health of Puerto Ricans or divert resources from their longstanding public health problems remains to be seen. Sharp recounted how members of dengue research teams were pulled off projects in order to help assess and quell the Ebola epidemic of 2013–16; for now, new resources and manpower have been diverted toward Puerto Rico to tackle Zika, but such reinforcements are rarely guaranteed
or permanent.
Dengue, a virus that infects an estimated 390 million people annually and kills about 22,000, is much like Zika in that it seems designed to haunt the contemporary hypochondriac:
While the disease shows classic warning signs—sudden, wrenching abdominal pain, a precipitous crash from fever to hypothermia, or shattering skeletal pains (hence its nickname, “breakbone fever”)—there are also asymptomatic infections, and plenty of cases that sound more like the unhappy amalgam of the flu and a hangover. Though dengue is an acute illness—quite possibly a one-off event for a precarious week or two—it is traditionally grouped into four serotypes, and infection with one does not confer immunity to the other three strains. In fact, evidence suggests that patients tend to fare worse with successive infections, with higher rates of mortality and conversion to the Ebola-like dengue hemorrhagic fever, rebranded in newer textbooks as the less evocative “severe dengue,” compared to dengue-naïve patients. So if you’ve had dengue once, a whiff of paranoia wouldn’t be entirely misplaced. Besides the obvious mosquito vector, it can be spread through blood transfusions or organ transplantation. After the acute phase of illness, some patients complain of joint pain, weakness, memory changes, and insomnia long after the virus has been cleared, though rigorous studies of such perceived aftereffects are still few and far between.
After the 2005 cluster of twenty-five confirmed dengue cases in the border town of Brownsville, researchers took blood samples from the surrounding community to see who else might have been exposed. Forty percent had antibodies against one or more dengue strains, suggesting that they had been infected some time in the past—if not during that cluster of cases, then at some other point, during which they may have simply written it off as the flu, food poisoning, or that most American of clinical ambiguities, a “bug.” Such missed cases are partly a comfort, in that they demonstrate how some people will take a dengue infection in stride. But these cases are part of what keeps dengue around: The mildly ill, out of the rarified wards of the hospital, continue to live among the world and its insects, getting bitten by Aedes mosquitoes that carry the virus to the next, possibly weaker, host—a newborn, an elderly parent, a chronically ill neighbor.
Puerto Rico is an island of 3.5 million people with a capital city, San Juan, comparable in size to New Orleans. It faces this illness year-round, every year, with upticks during the rainy season and major epidemics every three to five years over the past twenty-five. A recent epidemic in 2010 saw 26,766 suspected dengue cases, though these only count patients who sought testing and were subsequently reported, and some public health officials estimate the count was likely severalfold higher. Similar ambiguities shroud the island’s Zika count, which numbered 1,262 confirmed cases as of June 8, 2016.
The circumstances of Key West could not be more different from San Juan’s, though the path between the two cities can be neatly traced down the necklace of the Antilles. Key West is the southernmost of the Florida Keys, home to 25,000 people and host to 2.7 million visitors annually. Elizabeth Bishop, perhaps its best poet, described the place as “really awful” to her friend Robert Lowell—“always a mess, junky little boats all piled up”—then conceding in the same letter, “I like it very much.” This opposition of feeling seems characteristic of the town’s residents, who might volunteer by day at one of the Keys’ exquisite and irreplaceable wildlife refuges and come home to the first yawps of Fantasy Fest, the self-described “annual bacchanal,” at night. Or perhaps their tastes run conversely, and they could bear a couple fewer marsh preserves and a couple more bacchant-ready hotels, which in season have some of the highest occupancy rates in the country. Or, most commonly, they love and cherish it all, the Keys’ numerous contradictions spraying forth like its native bromeliad plants, waxy Technicolor rosettes beloved of the Keys’ mosquitoes and humans alike.
I spent a day with Dr. Mark Whiteside, the senior infectious-disease physician of the Monroe County Health Department in downtown Key West. Not long after we met, he drove me around town, pointing out the dive bars where he obliviated after-hours downtime in the years before marriage and, more importantly, showed me the blocks from which dengue fever radiated for an unsettling two years.
In 2009 and 2010, Key West recorded eighty-eight cases of dengue fever. The number reflected a tiny percentage of the population, but one that felt intimate and frightening in such a small and close-knit town. Early in the outbreak, random sampling of the town’s total population, sick and well, showed that 5.4 percent had serum evidence of recent infection—circulating antibodies to dengue virus indicating that it had resided in their bodies, whether or not it had been correctly identified at the time of onset. Mosquito control has been a high-priority conundrum since the Keys’ first human settlements, but this isolated dengue outbreak—there have been none since, nor any cases of Zika or chikungunya—was serious inducement to find new solutions. In those years, Whiteside saw dengue patients, helped the Florida Keys Mosquito Control District map affected hotspots, and wrote passionate editorials in the local paper about stanching the outbreak. Though the cameras have gone, Whiteside remains, and so does Aedes aegypti. He’s calling on everyone in town to “roll up their sleeves” and adopt the kind of “old-fashioned public health measures” that have typified his more than thirty-year career on the island.
AIDS was the disease that first brought Whiteside to Key West, which by the late 1980s had a higher prevalence of the disease than San Francisco, New York, or Miami. There are more than a thousand names on the town’s memorial—a staggering number for a town of about 25,000 residents. Whiteside moved from the Midwest to Miami in 1980 to pursue a fellowship in infectious disease, but his original interest in tropical diseases was quickly overtaken by the more urgent outbreak: a poorly understood syndrome that seemed to afflict gay men and a few other groups. Before AIDS was understood or even definitively named, Whiteside and a fellow physician drew up a constellation of signs and symptoms, so that if someone walked into a clinic with some but not all features of the syndrome, they could estimate the person’s risk of having the nameless disease and anticipate and possibly prevent some of the opportunistic infections that they knew were highly correlated.
Dengue, though less catastrophic, was Whiteside’s next opportunity to work on the front lines of an emerging disease, and he proudly showed me a folder of clippings and letters related to events of 2009 and 2010, including a catchy mnemonic he developed, “ABCD” (“Action to Break the Cycle of Dengue”).
Most importantly, he helped Key West bring down its Breteau index—the number of water-filled containers infested with mosquito larvae or pupae per 100 houses—from its 2010 rate of about twenty to less than five by 2011.
How is a Breteau index lowered? To find out, I visited the Mosquito Control District headquarters for Monroe County. One of the first things Beth Ranson, the district’s public education and information officer, handed me was a clear plastic bag full of brownish nubs that looked like Grape-Nuts.
The bits of feed corn were coated in a bacterium known as Bti, or Bacillus thuringiensisserotype israelensis, which wasdiscovered in a riverbed in Israel in 1976. The bacteria occur naturally in the digestive tract of several caterpillar species, much the way that many varieties of nonpathogenic bacteria inhabit the human gut. When Bti is sprinkled in standing water and subsequently ingested by Aedes aegypti larvae, however, the pH in the larval digestive tract causes the bacteria to release an endotoxin that crystallizes on the spot, forming a tiny obstructing stone that bores a hole in the larval gut.
The bacteria don’t appear to have this effect on any nonpest insects (though Bti also works on some caterpillars, gnats, and blackflies) or on fish or amphibians that swallow the dead larvae. It has not yet been detected in human drinking water, but it is believed to be safe for humans as well. The biggest theoretical risk to humans might be cross-contamination with pathogenic bacteria accidentally cultured alongside Bti, although production laboratories test batches for these tagalongs.
In both the Keys and Puerto Rico, the most visible and time-honored form of “vector control”—public health interventions aimed at stopping carriers of disease—is the spraying of wide tracts of land with so-called adulticides, which tend to be less species-specific in their ability to kill mature insects. In both places, trucks spray along designated routes, and this is complemented in the Keys by aerial spraying from aircraft. Environmentally sensitive areas are designated as “no-spray zones,” and schedules, published in the local newspapers, typically favor dawn hours with minimal human foot traffic. Still, nearly everyone I met in both Key West and San Juan had tales of rushing for cover when an unexpected spraying commenced, or recounted an ill-timed spray on a windy day that just might have drifted into one of the butterfly habitats or Key Deer refuges that are supposed to be off-limits.
Another problem with conventional vector control of mosquitoes is that routes relying on truck-based sprays miss the upper floors of multistory buildings. Dr. Jose Rigau-Perez, the former head of the CDC’s Dengue Branch in Puerto Rico, notes that he has found, and been bitten by, Aedes even in his tenth-story apartment, despite scrupulous attention to standing water and a better understanding of dengue epidemiology than almost anyone on the planet. The pesticide spray trucks that pass his building, in his opinion, are as much about “show[ing] people something is being done” as they are about efficacy. When I noted that finding Aedes in the home of the former Dengue Branch director is surely a sign that outbreak history is doomed to repeat itself, he interrupted me.
“This isn’t doom, it’s biology,” he said. “Because women have babies every day doesn’t mean they’re doomed to repeat history—it means we’re human. The mosquito is so adaptive to human environment that to be rid of them you would have to change the human environment so drastically, humans wouldn’t want it.”
In practice, though, mosquito-control organizations work daily to keep the mosquito population at a low smolder. In Key West, I spent an afternoon with Inspector Billy Ryan, an employee of the Florida Keys Mosquito Control District. A ruddy and gentle man used to working alone, he makes door-to-door sweeps of Florida Keys neighborhoods in search of mosquito colonies to target with the array of powders, sprays, and oils in his truck. He is also equipped with a notebook and an aging Palm Pilot with which to record the rough population counts he makes in the course of his day.
We spent an autumn afternoon focused on Water’s Edge Colony, a trailer park inhabited mainly by recent immigrants from Haiti and Cuba. Though governed by Key West, it’s on a separate landform called Stock Island, which accrued atop a coral reef alongside Key West, separated by the dainty Cow Key Channel. The poverty at Water’s Edge feels planets away from the jewel box of Old Town Key West: Individual lots are small, and the combined pressures to establish a sense of privacy and make room for one’s belongings encourages the production of idiosyncratic fortresses. Lots are delineated by disused porcelain toilets and sinks, bed sheets covered in cartoon characters, industrial plastic buckets, recycling bins, pink strips of insulation, and bamboo screens. Since Creole and Spanish are more in use than English here, and Ryan speaks neither, he keeps it simple. He issues a loud whistle when stepping onto a property and shouts hello as he raps the door. If someone emerges, Ryan’s standard gambit is, “You have plenty mosquito”—spoken as a declarative if he’s found them, as a question if he’s still looking.
According to Chapter 388 of the Florida Statutes, employees of Mosquito Control may enter and treat private property without the owner’s permission, but since trust and community engagement are major strategic assets, the inspectors avoid antagonism at all costs. Ryan doled out several dozen cat and dog treats in the course of the afternoon as he scanned for standing water, which he inspected with ladles and flashlights. Sometimes the households that have worked the hardest to convey a spirit of upward mobility are the ones with the most difficult mosquito problems: Larvae can breed in the thimblefuls of water that pool in the leaves of tropical houseplants, along the lips of birdfeeders, and in the crevices of Christian statuary. Lots studded with derelict washing machines and refrigerators are harder to miss. Ryan aimed his flashlight in the catchwater of a small bromeliad plant and showed me two tiny, dancing straws inside—mosquito larvae, periodically wriggling to the surface for air.
We drove a mile west to the nearby Sunset Harbor Carefree Manufactured Home Community. Though a bit more prosperous than Water’s Edge, the combination of its situation along Cow Key Marina and the season’s unusually high tides meant that many lots were soaked in brackish water. Hardly the next dengue or Zika hot spot—Aedes larvae prefer freshwater—mosquito eradication here diverts a frustrating amount of time and resources from more Aedes-friendly hot spots, since other mosquito species will happily thrive in the salty muck of Sunset Harbor and create a serious nuisance. For broad, inaccessible puddles such as the ones that accumulate under these trailers, the best option is to spray a thin sheet of oil across the top of the water, which suffocates larvae attempting to surface for air. The oil can evaporate in as little as twelve hours, however, which leads to a numbing repetition of this exercise if the tides and weather don’t change.
The rudimentary and repetitive nature of conventional mosquito control has long whetted the appetite of biotech entrepreneurs, who see an opportunity for both profit and public good. Ever since 1930s experiments into mating radiation-sick insects with healthy ones—which leads to sterile offspring, driving species toward extinction—scientists have sought the silver bullet that will curb mosquito populations without downstream ill effects for humans or other species. A fledgling UK biotech company called Oxitec, the modest startup of a few zoologists from Oxford University, has developed a radiation-free technique for genetically modifying Aedes aegypti mosquitoes such that their offspring would almost invariably die before maturity. In 2009—after the Keys’ dengue toll had begun but before the full scale of cases could be known—Oxitec and the Mosquito Control Board of Monroe County began discussions to make Key Haven, an unincorporated residential community a mile from Key West, the first site on US soil to release the genetically modified Aedes. The proposal unleashed years of heated public debate that remains unresolved. To date, Oxitec has already performed trials of its genetic biotechnology in small zones within the Cayman Islands (2009–10), Malaysia (2010), and Brazil (2011, 2014), but approval in the US, a highly lucrative and tightly regulated market, could be a bonanza both for this specific mosquito modification and for analogous genetic modifications the company might later develop to target other species or other traits.
The push for a quick solution to Aedes has never been more urgent: Human trials of vaccines and antivirals against dengue are currently underway, and the first vaccine against Zika could be ready to test on human subjects by late 2016, but even once available, such breakthroughs can require a decade of evaluation before their efficacy and sustainability in large populations is well understood. Yet the rise of Oxitec and genetic biotechnology does not thrill everyone. For instance, Mila de Mier, a realtor and entrepreneur in Key West who has become the de facto face of the anti-Oxitec movement, argues against what she sees as a deeply unethical attempt to conduct a quasi-medical experiment on a group of people who have not provided the individual informed consent that has become the hallmark of good practice in contemporary American science. (While the genetically modified mosquitoes are the direct subjects of the Oxitec trial, their release into human communities arguably makes residents part of the experiment, too.)
De Mier first read about Oxitec’s proposal to release genetically modified mosquitoes in her area nearly five years ago—when the specter of dengue still loomed large—and says she was initially enthusiastic about the project, until further research convinced her that the proposed genetic modification was dangerous and unnecessary. She created a Change.org petition on what she describes as a Saturday-night whim. The website asks petitioners to state a signature goal, and she fancifully wrote, “1500.” The petition surpassed that in a few days and now has more than 168,000 names from around the world. Media outlets took notice, and de Mier found herself juggling her real estate business, volunteer work at the local VFW, parenting, and animal care with phone calls from places like CNN and the New Yorker. She is ebullient and confident, and in the world of environmental and public health activism, she has become a minor celebrity.
“I’m a meat eater,” she told me bluntly, by which she meant that she considered herself a typical citizen. “I’m not anti-GMO, I’m not anti-anything. Don’t give me any tags, because I’m not.” The signatures on her initial petition, however, compelled her to accept a greater responsibility. Oxitec’s recent absorption into a larger, multibillion-dollar enterprise, Intrexon, which purchased the firm in 2015, has de Mier and others worried that the release of genetically modified mosquitoes in Key Haven is only minimally about Floridian public health. They believe that the project exists primarily to establish a legal and scientific precedent for the release of modified organisms into the US environment, which could then open the floodgates for a host of other, even more profitable projects. For de Mier, the current dynamic boils down to “risk versus respect”: Her sense that Oxitec’s and county officials’ willingness to undertake a project of unknown efficacy in her community signals a trifling valuation of the people who live there.
Heightening anxiety on both sides, the regulatory process has been at a near standstill for the genetically modified mosquito. Although the USDA initially considered Oxitec’s application in 2009, it eventually determined that, despite having approved superficially similar projects such as genetically modified fruit flies, it could not rule on the mosquitoes. A better fit, it said, would be the FDA, which entertains applications for “Investigational New Animal Drugs,” a power it has held since the 1938 Food, Drug, and Cosmetic Act. (Though the decision to legislate drugs and cosmetics together is reflective of early twentieth-century constructs of marketing and wellness, several Keys residents I interviewed also felt personally affronted and belittled by the Oxitec decision’s being subject to the same legislation as a “cosmetic.”) In March 2016, the FDA finally released its conditional approval for a field trial to release the modified mosquito, known as OX513A, in Key Haven.
The trial’s approval requires a sufficient period of “public comment,” which the FDA opened in March and closed in mid-May of 2016. Opponents have been scrutinizing the Draft Environmental Assessment submitted by Oxitec to the FDA. Oxitec explains their process as follows: Male Aedes aegypti are reared in a lab with three genetic modifications. The first, called tetO (tetracycline Operator), causes a second gene, tTAV (tetracycline repressible activator variant), to be “expressed”: in other words, for the protein it encodes to be built and released in great quantity within the cell. These two set up a positive feedback loop—tTAV causes more tetO expression, and vice versa—such that all of a mosquito’s transcriptional machinery (the process by which genetic blueprints are used to manufacture proteins) quickly gets tied up in making more and more tTAV protein. The mosquito cells are too busy making this junk protein to bother making the proteins they actually need, and the insect dies. As the expanded names of tetO and tTAV suggest, the antibiotic tetracycline serves as an “antidote” that inactivates this positive-feedback process. Modified mosquitoes are raised with a diet containing tetracycline so that they can survive long enough to be released into the wild, where they mate with the native female population, whose offspring inherit the feedback gene and, without access to tetracycline, die before maturity. A third genetic modification causes these mosquitoes to fluoresce in certain lighting conditions, so that modified mosquitoes can be distinguished from natural ones.
Critics of the OX513A plan see at least three potential pitfalls. The first is the tetracycline “antidote.” Tetracycline is a relatively old antibiotic from the 1940s, cheap because its patent has expired, and still sometimes used for infections such as chlamydia and everyday conditions such as acne, as well as in industrial livestock farming. Traces can be found in some pet food and in meat for human consumption. Since Aedes prefers living in human homes and yards, genetically modified offspring could theoretically access this incidental tetracycline that would allow them to survive and replicate, with unknown downstream effects on the ecosystem. However, Oxitec’s data show that the mosquitoes would have to consume many, many times more tetracycline-laced food than could be reasonably expected.
The counterargument, here and with other aspects of Oxitec’s data, is that the company’s findings have not been exposed to the dispassionate rigor that ideally takes place when scientists without conflicts of interest conduct a study and publish results in a peer-reviewed journal. Aspects of Oxitec’s technology have been vetted in peer-reviewed journals since as early as 2002, but Oxitec cofounder Luke Alphey is listed among the authors in almost every case. Because of the highly profitable and proprietary nature of its technology, Oxitec has no incentive to allow its data to be analyzed, or its methodology replicated and assessed, by an independent group any time soon—nor is it required to do so, since the FDA evaluates Oxitec’s mosquito plan largely on the self-stated merits that Oxitec enumerates in its Draft Environmental Assessment.
The second worry some critics voice is that laboratory error could cause some female mosquitoes—the sex that bites humans—to be sorted among males and genetically modified, thus releasing genetically modified creatures that are actually exchanging bodily fluids with humans. Oxitec acknowledges that a small fraction of female mosquitoes will inevitably be misclassified as male, but it also contends that no tTAV protein is present in mosquito saliva, thus reducing the risk of tTAV entering a human bloodstream. Again, de Mier and others are loath to accept data from company-funded and company-executed research.
Thirdly, opponents of Oxitec are concerned about a rigged scoreboard—if dengue hasn’t been documented in the Keys in six years, and Zika hasn’t yet arrived, how can we know whether genetically modified mosquitoes have an impact on human health and disease there? Or, if the primary metric of interest is mosquito population reduction, who is responsible for counting something as unruly and mobile as a free-ranging mosquito population? There’s no good answer to the first question. To the second, the Monroe County Mosquito Control District says that it will continue what it’s always done—track population trends by doing weekly counts of what flies into their mosquito traps, and conduct daily “landing counts,” whereby a mosquito inspector numbers the mosquitoes that land on him or her at a fixed minute each day. Both methods have their obvious imperfections—they’re contingent on everything from recent weather to employee attentiveness—but if conducted fairly and consistently over a long enough period, they provide valuable data over time.
There is, of course, no airtight rebuttal to the argument of unforeseen consequences. It’s always possible—perhaps even certain—that a technology will have ramifications we haven’t yet thought of. The degree of forethought and expertise that goes into creating a technology can perhaps give us a rough sense of how trivial or severe those phantom unknowns will be.
Michael Welber, a retired journalist and editor who lives mid-Keys in the town of Marathon, is concerned that public support for the proposed genetic modification project has been inflated. Inflammatory and emotional town- hall meetings have seemingly pleased no one, with participants saying their questions have gone unanswered and panelists saying their answers went unheard. Surveys are another way of assessing support, but Welber believes that the most commonly touted survey was invalidated by leading questions. The survey opens by asking respondents to rate the importance of mosquito control, then asks them to rate their agreement with the statement “Mosquitoes tend to be a nuisance where I live.” Respondents are then asked to choose “reasons why mosquito-borne diseases are limited in the Keys.” These early questions could be seen as priming respondents to feel favorably about the genetic modification initiative that comes up much later in the poll. To the poll writers’ credit, the genetic modification–related questions do contain multiple-choice options as to why respondents might fear or oppose the technology, such as “The genes inserted in mosquitoes will get transferred to other species and kill them too.” Welber still finds the document as a whole to be biased.
Perhaps the best indication of public support or opposition will be the 2016 local elections. The directorship and board commissioner positions of the Mosquito Control District are public offices. In those years when important state or national offices are up for grabs, the winners of local positions have received upward of 12,000 votes. During down-ballot years, turnout is so low that local positions can be had for less than 2,000 votes. So to some extent, the composition of the board is as representative as voter turnout allows. Several opponents of the Oxitec project invoked the concept of “informed consent” when they stated their most fundamental problem with the mosquito release. When I suggested the idea that a vote can serve as a proxy for group consent, I got one of two responses: Either voter turnout is too low to be a legitimate proxy, or even full voter turnout would be no substitute for the gold standard in contemporary science: obtaining the positive individual consent of each person who partakes in an experiment.
Puerto Rico’s own dark history of informed-consent violations strikes me as one reason why Oxitec may have avoided pitching a potentially controversial genetically modified mosquito trial there, even though its population is immensely vulnerable to Aedes-borne diseases. The intersection between Puerto Ricans and medical research has simply been too historically fraught. Perhaps the most notorious example dates to 1931, when the pioneering cancer researcher Cornelius Rhoads, then working in San Juan with funding from the Rockefeller Foundation, left a letter on his desk describing Puerto Ricans as “the dirtiest, laziest, most degenerate and thievish race,” adding that what the island needed was “something to totally exterminate the population.” To this end, Rhoads wrote that he had “done [his] best to further the process of extermination by killing off eight and transplanting cancer into several more.” Rhoads later claimed that the unmailed letter was intended as a “playful composition,” and a recent reinvestigation by a team of Yale University historians and bioethicists found the “confession” to be unrelated to actual deeds. Yet the language was clearly vile, and rumors continue to abound, with elaborate internet speculation about clinics in which Rhoads purportedly injected cancer cells into unwitting victims.
Less rhetorically sensational but as damning were early trials of oral contraceptive pills in the 1950s. Drug developers needed a large human trial to demonstrate safety and efficacy, and considered Puerto Rico—where tubal ligations and abortions were already relatively common—to be more culturally receptive to the new drug than anywhere else in the US. An initial pill prototype with a high dose of progesterone (quite different from most current formulations, which combine low doses of progesterone and estrogen) was distributed to thousands of Puerto Rican women, nearly 20 percent of whom experienced severe nausea, vomiting, mood changes, and other side effects. Three women died, likely due to secondary blood clots that can also be a deadly effect of estrogen and progesterone combinations. None were informed that they were participating in an experiment with an unapproved drug.
CDC Lieutenant Commander Tyler Sharp calls such historical episodes “horrid and shameful” and a “black mark on our record.” He remains respectful when locals joke about the nefarious things he might be up to, or opt out of the studies or routine surveillance that his office conducts. The very correct circumspection that Sharp and his colleagues favor, however, may be one reason that the bulk of cutting-edge dengue interventions generally happen in places other than Puerto Rico.
Then there’s Puerto Rico’s shortage of resources and manpower, which hinders everything from everyday medical care to the more elaborate health surveillance that’s needed for large-scale clinical trials or in case of epidemics. On average, a doctor left Puerto Rico every day in 2014; the incentives to stay simply aren’t strong enough. Without those clinicians, Sharp says, “we lose our eyes and ears” on the front lines of public health—and communities lose some of their most needed and trusted members.
This brain drain is partly a consequence of the island’s darkening economic picture. Puerto Rico became a favored site for American industry thanks to the 1976 Possessions Tax Credit (known as “Section 936”), which offered tax exemptions on income in Puerto Rico and other US territories, in part as a political move to keep US-affiliated markets stronger in the Caribbean and Latin America than more leftist governments in the region. These exemptions, plus a proud history of Puerto Rican university training, lured multiple pharmaceutical companies to the island. When mainland US political winds shifted in the 1990s to focus on paying down the federal deficit, austerity measures were handed to the island from the outside, and Section 936 was phased out by the Clinton administration.
Though the island has been steadily defaulting on slivers of its $72 billion debt, Chapter 9 of the US Bankruptcy Code does not delineate a specific process whereby a territory outside the fifty states can declare bankruptcy. (A June 2016 Supreme Court decision ruled that Puerto Rico does not have the right to design the restructuring of its own debt, as it had previously attempted to do, without prior congresssional approval.) Because of this state of limbo, a somewhat improvisational spirit seems to have overtaken the US Congress with regard to Puerto Rico’s finances, including proposals to sell off protected wildlife habitats to private investors.
Puerto Ricans’ gains and losses depend largely on policies that they do not write or vote on. They also depend on the equally undemocratic forces of nature: last year, an island-wide drought forced some of the toughest water restrictions in contemporary American history. At its nadir, San Juan residents had running water one day out of four. The 2015 Puerto Rican drought did not earn an article of its own in the nearby Miami Herald, which ran several dozen stories about the Californian drought the same year.
For now, the mood in Key West is far sunnier, with no known cases of Zika and a temporary closure of community fault lines while the FDA evaluates the materials it received during the spring 2016 public comment period on the Key Haven project. Mark Whiteside took me birding at Fort Zachary Taylor State Park. Driving along the park’s single-lane road, he stopped so that a butterfly could continue on its path. To challenge himself and make the most of his often short periods of time away from his clinic, he invented a game he calls “power birding,” the goal of which is to try to find as many unique species as possible in an hour. During our own power birding session we saw about twenty—a bad day, in his book—but I was less impressed with the parula or the sharp-shinned hawk than I was with Whiteside’s patience and passion for accuracy. He reminded me of Key West part-timer Wallace Stevens, whose poetry ends many places but always starts with what’s actually there. Stevens’s “Study of Two Pears” famously concludes, “The pears are not seen / As the observer wills.” Good science and good poetry both begin in good faith and a dislike of charlatanry.
Seventeen miles north of Key West, in Sugarloaf, stands Perky’s Bat Tower, a cypress structure reminiscent of the chicken-legged house in the Baba Yaga fairy tale. It is said to have cost $10,000 to build in 1929 (nearly $140,000 in today’s dollars) and was loaded to the gills with highly aromatic guano, all to attract hordes of bats that would end the problem of mosquitoes and the viruses they carry. No bats arrived. The smell was said to be terrible. Just offshore to the west sits Fort Jefferson, 16 million bricks big and the largest masonry structure in the Americas, conceived during the Napoleonic Wars and fitfully built throughout the nineteenth century before it was abandoned in the 1880s. Hunches that it would occupy a critical position in the Napoleonic Wars, then the American Civil War, were never borne out. Like any region, the Keys are rife with monuments to over- and mispreparation. It is just possible that the mustering of genetic biotechnology to avert viral outbreaks may face a similar fate.
Still, if the Oxitec project goes forward with the consensus of the local public, the potential benefit to the larger global community could be enormous. The cost of rejecting this technology, if a better option fails to materialize, could on the other hand be unspeakably tragic for pregnant women and others who bear the brunt of Aedes-borne epidemics of dengue, Zika, and chikungunya. Data on the success of the OX513A vector-control project would be valuable for human health worldwide: Although Oxitec has already published data on its genetically modified mosquito releases in the Cayman Islands, Malaysia, and Brazil, a trial on American soil would, rightly or wrongly, generate far more scrutiny and discussion than trials in parts of the world that go relatively unseen by the developed world.
And in Key West, such data would be uncommonly clean—relatively free of excess variables that might skew or muddle a study’s outcomes—which, in the world of scientific method, correlates directly to a study’s credibility. Key West and Key Haven have small landmasses, small year-round human populations—particularly during the rainy mosquito-breeding season—and one road in. Compare this with a bustling tropical city such as Rio de Janeiro or Ho Chi Minh City, Vietnam, where the release of a modified mosquito could potentially avert thousands more illnesses; but in the chaos of variables that confound every metropolis, who would ever know?
In other words, the best argument for Keys residents to support Oxitec’s Key Haven trial may be altruism. Zika has not arrived and hopefully never will; the last outbreak of dengue lies six years behind them. Yet mosquito-borne illnesses afflict swaths of the world on a near-permanent basis, and data derived in Key Haven could come to the aid of San Juan and beyond. The US has already seen three cases of Zika-attributed microcephaly—one each in Hawaii, New Jersey, and Puerto Rico. Surely this is three too many.
Parts of America wait for the public health they need, virtually invisible to most news outlets and their audiences, most politicians and their constituencies. While they wait, they make do with what they can. These pockets of invisibility may be deep in the park you run laps around, or in the emergency room you pass on the way to work. They may have had names that now appear on an AIDS or a yellow fever memorial. They may be entire provinces or islands. “Why is the Puerto Rican population not seen as Americans? Why don’t they matter?” Sharp asks, angrily. There’s no good answer—certainly not the cold comfort that there are many half-forgotten places. For now there’s just the lukewarm comfort that help—in the form of vaccines or genetics—may be months away, if they can only wait.



No comments:
Post a Comment